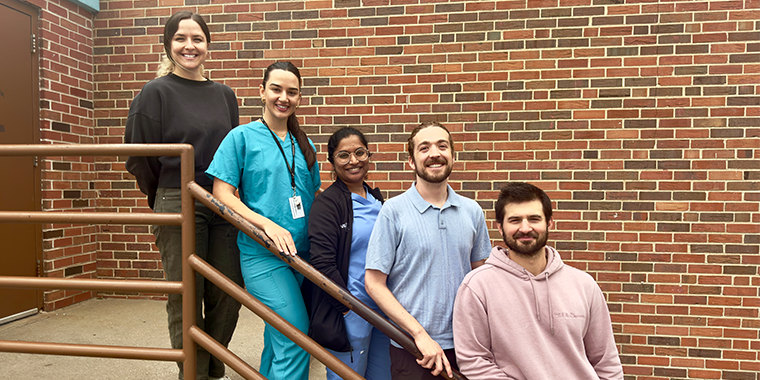
For newly arrived refugees, the American health care system can feel like a maze without a map. A partnership between Kansas City University’s (KCU) Center for Population Health and Equity and Della Lamb Community Services is helping to change that. Through the Refugee Health Navigator Program, second-year osteopathic medical students at KCU are paired with refugee families to offer steady support to help them become self-sufficient in their health journey.
Each team includes one male and one female student doctor, offering both cultural sensitivity and consistent advocacy. Inspired by a model from Georgetown University, the students act not as clinicians, but as trusted guides—helping clients schedule appointments, manage medications and access essential services like transportation and insurance.
What’s emerging is more than better access to care. It’s a powerful model of community-based support that empowers refugee families and prepares future physicians to lead with empathy and cultural awareness.
Building trust one barrier at a time
For Lejla Hodzic and Elliot Parens, building trust was the foundation of their work. Hodzic, the daughter of refugees, brought a personal understanding of the invisible barriers their clients faced, language, transportation, paperwork and the stigma surrounding mental health.
“Refugees are intelligent and resilient,” Hodzic said. “They’ve overcome unimaginable barriers. Now more than ever—amid shifting policies and uncertainty—volunteer programs like ours are essential for helping refugees navigate the complex U.S. health care system and adjust to life in a new country.”
Parens was drawn to the program because of its long-term, relationship-centered approach. “This is about providing real service,” he said. “Not just what we think they need.”
Together, they helped their client family gain access to overlooked areas like dental care, while slowly opening space for deeper conversations around mental health and preventive care. With consistent support, the family learned to navigate the system more independently.
“Medicine isn’t static,” Parens said. “It’s always evolving, and policy directly impacts people.”
Creating space to be heard
One student team worked with a refugee woman who was hesitant to speak openly about her health. Pooja Gunnala’s presence as a female medical student helped create a safe and trusting environment.
“Refugees often feel pressure to appease,” Gunnala said. “That creates real gaps in communication.”
Together with her partner, Mason Tuttle, the team tailored their communication strategies. They verified interpreters were using the correct dialect, texted directly when language services weren’t available and used teach-back methods to confirm understanding.
“We do a lot for them,” Tuttle said. “But we explain everything so they can eventually do it themselves.”
As trust grew, so did their client’s confidence, asking more questions, voicing concerns and advocating in medical settings.
“It’s been a humbling experience,” Gunnala reflected. “Small adjustments from providers can make a big difference in outcomes.”
A life-saving lesson in listening
When Kathleen Parens and David Fanous supported a client during a hypertensive emergency, they had to act quickly. Though not providing direct medical care, they recognized warning signs and ensured their client received prompt attention.
“In the moment, it was instinctive,” Fanous said. “We asked simple questions—do you have a headache? Blurred vision?”
The crisis marked the beginning of a deeper relationship. They began supporting the client’s primary medical team by helping track the client’s blood pressure, reminding her about medications and coordinating follow-up care.
“Every time I call, I ask how her blood pressure is,” Fanous said. “If it’s high, we make a plan.”
Fanous, a native Arabic speaker, also faced unexpected challenges with dialects. “Sometimes what I say doesn’t land the same. But their questions teach me. They help me think differently.”
Parens agreed. “You can’t assume understanding. Being present and listening is where care begins.” she said. “This work is about meeting people’s needs, not just our growth.”
A shared journey toward independence
This pilot program has already evolved into a model that addresses critical gaps in refugee care while shaping a new generation of culturally aware physicians.
“We really need more support to come around these individuals and families to help them navigate their challenging health issues,” said Ellie Colvin, refugee services coordinator at Della Lamb Community Services. “The goal of this program is to empower refugees to become self-sufficient in their health journey and beyond. It’s about giving them the tools to access care independently, while shaping future doctors who understand that care goes far beyond the exam room.”
These student doctors have not only shown refugee families that they don’t have to find their way through the system alone, but they’ve also gained a deeper, more holistic understanding of health care, one that will shape the way they practice medicine throughout their careers.
To learn how a refugee KCU alumni family built a remarkable medical legacy, click here.


_20240320154858_0.png?w=140&h=140)
(0) Comments